It’s a bit of a sticky wicket. There are a handful of vendors out there that offer cloud-based storage and transfer. The basis for their existence is to offer cloud storage for patients, so that they can share their imaging with all of their doctors. These vendors offer this at a charge for retention.
To make this process work, they need the ability to get these images from hospitals and clinics. So usually a hospital will sign up with one vendor and for a fee, enable other hospitals to receive their images. So the hospital now spends money on sending images to the cloud instead of burning cds and mailing cds out. That hospital then reaches out to the other hospitals that typically receive cds from the sending hospital and enlists them as a user. The user will receive these image transfers at no cost but will be charged if they forward those images to another facility. So you can see, this was built to replace cds but made the hospital build a client base.
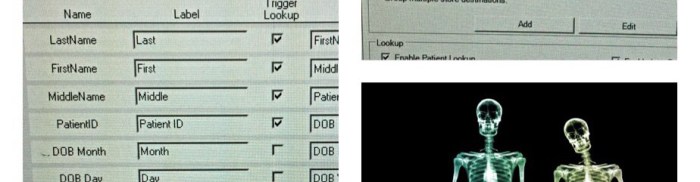
As it turned out, not many hospitals actually enlisted their patients to sign up for this service. It became a useful product to send images to frequently used facilities like MD Anderson and Mayo Clinic. It became the norm to send conference images like Tumor board or Chest board via these shares. Most hospitals would take these exams and load them directly into their PACS when received, cutting down on the time it took to import from a cd.
So here we are back to the list of vendors. Not every hospital uses the same vendor or shares the same cloud space. The products we use are what we use. What ABC hospital or DEF clinic uses is their choice. What iConnect or CHAShare provides is a way of sharing our images with other facilities with their own login and password to access our cloud for our images. All of the vendors offer this, so in some form or fashion, we should be able to set whomever we want up to do the same thing as ABC hospital.